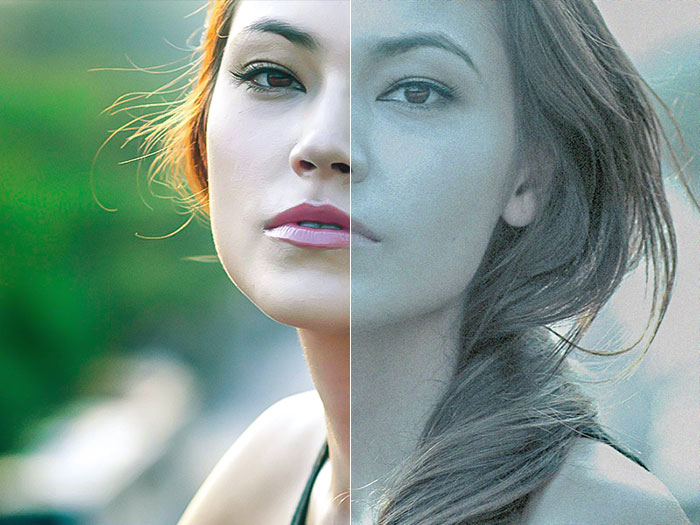
Send us your photo
We do the magic and print
Receive package up to 48h
Introduction
Living with a leg injury can considerably impede one's mobility and independence, thus rendering even the simplest of tasks challenging and fraught with discomfort. However, there exists a solution that holds the promise of restoring freedom and alleviating discomfort for those with such injuries: a rollator walker with a seat. This versatile mobility aid seamlessly integrates the convenience of a traditional walker with the added advantage of a built-in seat, providing a resting place whenever required.
With careful regard to the needs of individuals with leg injuries, rollator walkers with seats have been thoughtfully devised. These walkers serve as dependable and steady modes of transportation, enabling individuals to navigate their surroundings more efficiently and with reduced exertion.
Understanding Rollator Walkers with Seats
A rollator walker with a seat is distinguished by its ability to cater to the unique requirements of those with leg injuries. Ascertaining smooth traversal, these walkers employ robust wheels that facilitate seamless movement across a range of terrains. Whether indoors or venturing into the open, a rollator walker with a seat engenders stability, lending confidence to sustain an active lifestyle.
Enhanced Mobility
Among the most noteworthy advantages inherent in employing a rollator walker with a seat lies within its ability to augment mobility. The presence of a leg injury engenders hardship, transforming even the most rudimentary of tasks, such as walking or remaining upright for extended periods, into onerous endeavors fraught with agony. However, employing a rollator walker mitigates these tribulations.
The wheels adorning a rollator walker facilitate enhanced maneuverability and ease of motion. By endowing a smooth and gliding gait, these wheels alleviate strain upon the injured leg while endowing requisite support to maintain equilibrium and steadfastness. Be it maneuvering through restrictive spaces or surmounting uneven ground, a rollator walker with a seat empowers individuals, allowing them to saunter assuredly and with grace.
Comfort and Support
Rollator walkers with seats confer yet another indispensable benefit through their emphasis on comfort and support. The experience of living with a leg injury typically births discomfort, pain, and fatigue. A respite becomes imperative, prompting the introduction of a built-in seat that invites rest whenever required, thereby mitigating strain incurred by the injured leg.
Moreover, the inclusion of a backrest within rollator walker with seat ensures optimal comfort and buttresses posture. This fortifying attribute consolidates the overall stability of the walker, thus facilitating snug seating arrangements while simultaneously maintaining proper spinal alignment. Owing to these supportive and restorative provisions, rollator walkers with seats assuage myriad adverse effects that leg injuries may impose upon one's day-to-day activities.
Convenience and Independence
Rollator walkers with seats transcend the realms of mere mobility and comfort; they exemplify the epitome of convenience and independence. Connoisseurs of practical design, these walkers possess an array of user-friendly features aimed at facilitating one's daily life.
Sundry rollator walkers with seats feature built-in storage compartments or baskets, affording individuals a haven in which to store essential items like water flasks, personal belongings, or even provisions. Liberated from the need to rely on extraneous bags or the assistance of others, independence flourishes, and self-reliance is fostered.
Furthermore, select rollator walkers come replete with additional amenities such as trays or holders designed to accommodate refreshments or reading materials. These thoughtful conveniences permit the indulgence in a meal or the pursuit of leisure activities without necessitating departure from the secure confines of one's respective walker.
Choosing the Right Rollator Walker with Seat
When endeavoring to secure a rollator walker with a seat, prudent consideration of several key factors is essential:
- Adjustability: Ascertain that the walker's height may be readily modified to align with your specific needs. This ensures proper posture alignment and affords comfortable usage.
- Weight Capacity: Meticulously verify the weight capacity of prospective rollator walkers to guarantee optimal support consonant with your physique. It is imperative to select a walker capable of accommodating one's individual requirements.
- Brakes: Displaying discernment in the selection process necessitates availing oneself of rollator walkers endowed with dependable braking systems. Such brakes confer the invaluable boon of enhanced safety, particularly when navigating sloping terrain or traversing uneven surfaces.
- Portability: The weight and foldability of a given rollator walker merit careful contemplation. Portability is of the essence, as it affords effortless conveyance from one location to another, engendering convenience at all times.
Conclusion
As a portentous conduit capable of eclipsing imposed impediments to mobility and independence, a leg injury comes fraught with challenges. Nevertheless, with suitable assistance and support, such challenges may be surmounted. A rollator walker with a seat stands as a testament, showcasing a practical and efficacious solution that enables individuals with leg injuries to regain their freedom and alleviate discomfort.
The enhanced mobility, comfort, convenience, and independence that rollator walkers with seats confer serve to engender a existence teeming with fulfillment and gratification. By adhering to the meticulous process of selecting a rollator walker with a seat tailored to one's unique needs, and harnessing the full range of features at one's disposal, daily tasks may be confidently undertaken, thus heralding a reinvigorated life abundant with activity. Do not allow a leg injury to serve as a sentinel of confinement—embrace the panoply of benefits proffered by a rollator walker with a seat, and verily reclaim the mantle of mobility.